elder
Depression is NOT inevitable in older life.
 Our youth-oriented Western culture seems to tell us that we are all doomed to succumb to debilitating depression as an inevitable part of growing older. This is not true!
Our youth-oriented Western culture seems to tell us that we are all doomed to succumb to debilitating depression as an inevitable part of growing older. This is not true!
Sure, it is true that getting old “ain’t for sissies” as Bette  Davis famously put it. There are a myriad of challenges that confront us. Nobody would argue that! We know what those challenges are – all kinds of changes, losses of various sorts from little things to profound ones, aches and pains, the gamut.
Davis famously put it. There are a myriad of challenges that confront us. Nobody would argue that! We know what those challenges are – all kinds of changes, losses of various sorts from little things to profound ones, aches and pains, the gamut.
But, you can also thrive in later years. It’s about your mindset, your emotional and spiritual practices and your strong support network. The kids called support networks these days, their “posse”. Your posse can be made up of old and new friends, your peers, support group members, family, pets, counselors, trusted doctors and spiritual advisors.
Generally, people like you have an assortment of healthy, tried-and-true coping skills that have gotten you this far in your life. Perhaps now, however, you are encountering an accumulation of situations that tax those skills. It may be time to remember your old skills and to learn new ones. It may likely be time as well to rethink your life’s purpose. Purpose is key to keeping your mood up and your heart content.
What stands in the way? Well, too many times, that old Shame rears its head and tells you that you ought to be able to figure this out on your own, that you ought to be able to just “tough it out” and do it alone or else you’re weak. You can’t burden your children so what to do? As the blue box here says, don’t keep it bottled up inside!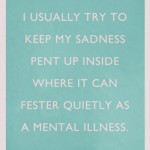
What people often don’t realize is that you are not alone in feeling challenged, stressed, confused, overwhelmed or anxious. These feelings surface when we are going through new phases and transitions in our lives. It’s during these times that it becomes so important to realize you don’t have to reinvent the wheel. There are many practices and tips for how to increase your enjoyment of life in older years.
The important thing is to not give up and figure that just depression goes with the territory. That may be what society tells you, it might be the prevailing attitude. But it is not true. Reach out for help. Counseling and support can turn your life around and help you reclaim your confidence, solid footing and peace of mind. Isn’t it worth a try? What have you got to lose!
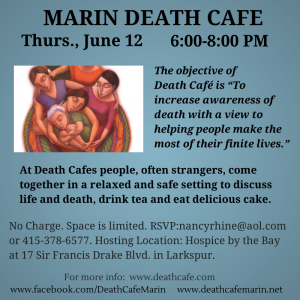
June 12 Marin Death Cafe
It’s Vital to Recognize Depression in Aging Adults
This is a very good, short article on why it is so important to recognize the signs and symptoms of depression in older people. They may not recognize that they themselves are depressed so it is imperative for caregivers and loved ones to be on the lookout. Undiagnosed depression can lead to isolation and even suicidality. Most cases of depression can be cured. This article is written by an older gentleman who has over 30 years experience working in retirement community and health facility administration. He includes reminders and tips for fighting depression in this article. Recognize Depression in Older People – You May Save A Life
Older Adults in Mill Valley
As Mill Valley Commissioner on the Marin County Commission on Aging, in October 2009 I presented my annual report to the Mayor and City Council members on the status for baby boomers and older adults living in Mill Valley. Here is a link to my report presentation notes – I hope you will find it helpful to give you an idea of some of the opportunities and challenges for older people in Mill Valley as of autumn, 2009. Some things have changed – statistics, numbers, contact information perhaps, so do note that this report is from 2009. Older Adults in Mill Valley
Fall Prevention
Fall Prevention. Falls are a high priority concern for middle age and older people since they are at increased risk for bone fractures and other fall-related injuries. Using a cane or eventually a walker helps many individuals to be steadier and more confident while walking. Some of the reasons, clients cite for falling are: tripping on something, their legs just “giving out”, and feeling dizzy. One often overlooked cause of unsteadiness and lightheadedness is dehydration. As we age, our sense of thirst tends to decrease – so it is important that we consciously make sure to drink plenty of water every day. An easy way to help fight the dehydration that can occur over the course of the night is to keep a glass of water on your night stand. When you wake up, sit up and drink the water before getting out of bed. Also, squeezing your calves and circling your ankles *before you get out of bed* will help increase your lower body circulation and make you feel steadier when you do get up and on your feet. For more fall prevention tips, check out http://www.mayoclinic.com/health/fall-prevention/HQ00657 .
Butler’s 3 Consequences of Ageism
From AgingWatch.com. Aging Watch is an independent think-tank committed to ending ageism and the social marginalization of older people.
————————————————————–
In 1969, Dr. Robert Butler coined the term “ageism” to describe this process of systematic stereotyping and discrimination against older persons. The three most devastating consequences of ageism include:
- The underutilization or exclusion of older peoples’ knowledge and insights in our civil discourse.
As a result of the negative stereotypes associated with growing old, elders are consistently responded to with sympathy and pity—often in the form of charity. While certainly well intentioned (and beneficial for many), this sympathy is a double-edged sword; the kindness it elicits is dripping with condescension and paternalism. Many elders are treated as vulnerable children in need of our protection and good will. And like children, the knowledge, voices, desires, concerns, choices, contributions, and opinions of elders are often devalued or dismissed altogether. “If older people are incompetent has-beens who lack self-sufficiency,” so the thinking goes, “then what could they possibly have to add to our society?” The result is that the vast knowledge and social contributions of older people are overlooked and squandered. - The poor and unfair treatment of older adults that stems from age biases.
Much like racism and sexism, ageism is a social disease that paints older adults as an “other” and fosters differential (and often unfair) treatment in many areas of life. In the workplace, for example, older job applicants are less likely to be hired, and are viewed as more difficult to train, harder to place into jobs, more resistant to change, less suitable for promotion, and expected to have lower job performances. Older workers typically suffer extended periods of joblessness after being laid off, and when they do find work, it is often at salary levels far lower than what they have earned in the past. According to the Equal Employment Opportunity Commission, age-based discrimination complaints in the workplace are currently at an all-time high. - The assault on older individuals’ identities and self-esteems.
In social interactions older people are assumed to be slow, weak, and forgetful. Researchers have documented the propensity of younger individuals to use “baby-talk” (i.e., exaggerated tone, simplified speech, and high pitch) when speaking to older adults. Elders are at risk of internalizing these low expectations, which can then lower self-esteem and foster bitterness and disillusionment. Instead of coming in contact with the harsh judgments of others, some elders become reclusive and completely withdraw from society; they become socially isolated and put themselves at increased risk for negative health outcomes (including depression, alcohol abuse, and suicide).
By addressing ageism and transforming the way our society sees older people we can appreciably enhance the lives of elders; and our social debates can benefit from an increased presence of elder wisdom.
Fixing US Health Care by Ken Dychtwald
How do we make sure that our older citizens are taken care of vis a vis health care and health care reform? Ken Dychtwald has some ideas in this thoughtful article. -NR